MOHS SURGERY
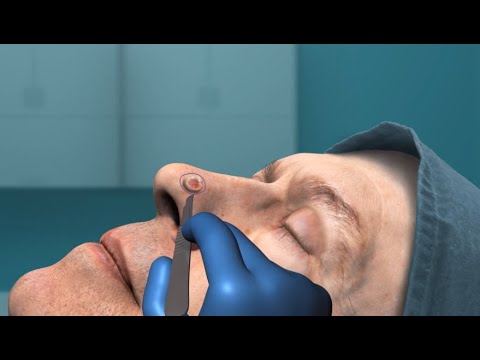
The process of Mohs micrographic surgery was created by Dr. Fred Mohs when he was a medical student over fifty years ago. He developed a meticulous and precise surgical technique used for removing skin cancers. This procedure has gained wide acceptance for skin cancer treatment in the last twenty years. The name micrographic comes from micro, indicating the use of a microscope, and graphic, indicating that a detailed map or drawing of the tumor is made during the treatment.
MOHS SURGERY REQUIRES THE FOLLOWING THREE STEPS:
1. Remove the visible tumor to determine the initial tumor borders.
2. Remove a thin disk of skin around and underneath these borders.
3. Examine the removed skin under the microscope and draw a map of where skin cancer remains.
If cancer is still present, we will pinpoint the location and remove only that skin where the cancer remains. These steps are repeated in cycles until the tumor is totally removed. In this way, a careful, accurate and complete removal of the skin cancer is achieved with minimal removal of normal surrounding skin.
To see a video presentation about MOHS SURGERY please click on video below.
ADVANTAGES OF MOHS MICROGRAPHIC SURGERY
The Mohs technique has a number of advantages over other methods of skin cancer treatment because no guesswork is involved. The microscopic analysis allows us to remove only those structures involved with the cancer. In other words, the cancer is completely removed while normal tissues are conserved. This procedure results in the smallest possible tissue defect and therefore, the smallest possible scar.
In addition, the surgeon acts as the pathologist and immediately examines the removed tissue. The surgeon can directly compare what is seen on the patient's skin to microscope slides. This is not the case when tissue is sent to an outside person for interpretation.
The Mohs technique provides cure rates for primary (previously untreated) and recurrent (previously treated) basal cell and squamous cell cancer of 94%-99%. The cure rate varies depending on the type of cancer and the type of treatments already performed.
WHAT TO EXPECT BEFORE SURGERY
The team will review your medical and surgical history, drug allergies, and your medications to ensure a smooth surgical procedure. This is often best accomplished beforehand with a consultation to plan the surgery and post-operative care.
Your skin cancer surgery will be performed in an outpatient surgery unit with local anesthesia. Hospitalization for Mohs surgery is rarely required.
To decrease your risk of infection, please shower the morning of surgery and wash the surgical site thoroughly. Wear comfortable clothing.
While your surgery will be completed as quickly as possible, you should plan to spend the whole day with us. Most patients are here for 4-6 hours.
Things to bring with you:
1. Complete list of your medications
2. Reading materials
3. Snacks and/or lunch
4. Computer (We have free Wi-Fi)
5. A fleece or extra layers to keep warm
6. Cell phone or other music device with headphones
WHAT TO EXPECT DURING SURGERY
Our staff will prepare you for surgery by taking your vital signs, checking your medications and medical history, photographing the skin cancer, and obtaining your signed informed consent for the surgery.
We will then cleanse and numb the area using a local anesthetic. Surgery will begin with the removal of a small piece of skin including the cancer. Any bleeding will then be stopped and a bandage applied to the area.
You can relax in your private room or in the waiting room while the tissue is processed for microscopic examination by the surgeon.
If the microscopic examination shows persistent cancer, an additional stage of surgery will be necessary. On average, Mohs surgery requires two or three stages to completely remove the skin cancer.
Once the cancer is removed, we will discuss your options for managing the surgical wound. In most cases, we will proceed with the reconstruction immediately. On occasion, special arrangements will need to be made for your reconstruction.
WHAT TO EXPECT AFTER SURGERY
-
During surgery, pain is prevented by the use of local anesthetic injections. Typically, the anesthesia loses its effect 3-6 hours after surgery is complete. Tylenol alone usually takes away further pain.
-
Great care will be taken to seal all blood vessels during surgery, and a pressure dressing will be applied before you leave our office. These two measures should prevent any significant bleeding. Occasionally, post-operative bleeding occurs. Those individuals who are on blood thinners, drink alcohol before or after surgery, or who stretch or traumatize the wound within the first few days after surgery may be more prone to this type of bleeding.
If bleeding through the pressure dressing occurs, apply firm, even pressure with your hand for a full 20 minutes. If this does not halt the bleeding, call our office at (650) 326-7222 or go to the nearest emergency room.
-
Bruising around the operative site is common. These will disappear similar to other bruises. The eyelids and cheeks are particularly sensitive. Bruising of one or both eyes may occur, even when they are not directly involved with the surgery.
-
All wounds will have some drainage. This should steadily improve each day. Increasing drainage can be a sign of infection.
-
Any time the skin is broken, by trauma, surgery, or other causes, an infection is a risk. Fortunately, close attention to wound care largely prevents infection from occurring. Non-infected wounds will gradually become less red and less painful each day after surgery. Infection is signaled when redness and pain increase. If you suspect an infection, call us immediately. Infections are treated with antibiotics.
-
One can expect some swelling (edema) the week after surgery. Swelling will be worst the first two to three days after surgery and should gradually resolve. Applying ice and sleeping with the surgical site elevated is helpful in minimizing post-operative swelling.
-
It is normal for surgical wounds to become red. The redness is part of normal wound healing. Increasing redness spreading out from the wound can be a sign of infection or an allergic reaction. If you suspect a problem, please call our office.
-
Scars always result from surgery of the skin. Our intent is to minimize the scarring and provide the best possible cosmetic outcome. Scars continue to heal and mature for 12-18 months after surgery. On occasion, a second procedure can help disguise the scar further.
WOUND CARE
After a Mohs surgery procedure, most patients find the recovery process simple and easy thanks to the streamlined surgical approach that leaves surrounding tissue unharmed. Nonetheless, it's common for patients to wonder what they can expect after a Mohs skin cancer surgery. This video is intended to help you understand what to expect in the short and long term.
FAQ ABOUT SKIN CANCER
-
Cancer is unregulated replication of cells that our bodies cannot stop. As the cancer cells replicate, they form a tumor. It is this tumor which invades and damages your normal healthy tissue. The most common cause of skin cancer is long-term exposure to sunlight.
-
The most common skin cancer is basal cell carcinoma (accounting for 80% of skin cancers) which arises from the cells on the lowest layer of the epidermis. The next most common skin cancer, squamous cell carcinoma (16% of skin cancers), is derived from the epidermal cells (keratinocytes). Melanomas, which account for only a small percentage of skin cancers, develop from melanocytes, the cells that produce pigment in your skin. Many people wonder if basal cell carcinomas can progress to melanoma. You can be assured that cancer of one cell type does not transform to another cell type – that is, basal cell carcinomas do not “become” melanomas.
Basal cell carcinomas almost never spread (metastasize) to distant parts of your body. However, certain squamous cell carcinomas do have a higher risk for spreading. Risk factors include the size of the tumor, the location, and whether your immune system is suppressed.
There are also subtypes of basal cell and squamous cell cancers. Some remain on the surface of the skin, while others can form “roots” underneath the skin. Therefore, what you see may only represent a small portion of the tumor that needs to be removed. We distinguish the different cancer subtypes with a skin biopsy and examination under a microscope. It is important to diagnose the cancer subtype so that we can advise which treatments are best for you.
-
Skin cancer is the most common form of cancer in humans. Over 2 million new cases of skin cancer will be diagnosed this year in the United States.
-
The treatment of skin cancer has four goals:
1. Completely remove the cancer
2. Preserve normal skin
3. Preserve function
4. Provide an optimal cosmetic result
-
Dermatologic surgery is a subspecialty recognized by the American Medical Association dedicated to the diagnosis and treatment of medically necessary and cosmetic conditions of the skin. The purpose of dermatologic surgery is to diagnose and remove skin cancer but also to reconstruct (repair) and/or improve the function and appearance of skin tissue.
-
A Mohs/dermatologic surgeon is a board-certified dermatologist who has undergone additional extensive fellowship training to become an expert in Mohs micrographic surgery, reconstructive surgery, and cosmetic procedures.
FAQ BEFORE SURGERY
-
No. We recommend that you eat breakfast and take all of your normal medications. There are no dietary restrictions but we suggest that you refrain from drinking alcohol for 2 days before and after your surgery. Alcohol thins the blood and increases your bleeding risk.
-
The doctors use local anesthesia only. You will not be sedated during the procedure. In most cases, the anesthesia is exactly the same used during the biopsy.
-
Given that Mohs surgery occurs in stages, we never know exactly how long you will be here. On average, patients are here for 4-6 hours. (If you are scheduled for an excision and NOT Mohs surgery, plan on 45 minutes.)
-
Yes! We have complimentary wi-fi and you are welcome to bring your laptop. Cell phones do not interfere with our surgical equipment and can be used while you wait between stages.
-
This depends mostly on the site of your surgery. You will not be sedated so mentally you will be able to drive. However, if the site is near your eye (including upper cheek and nose) the post operative bandage may obstruct your vision especially if you wear glasses. Other examples include a surgery on the neck which may make it difficult to turn your head while backing up a car, or a surgery on the foot which may prohibit you from operating the vehicle. If you have any questions, please ask us when you schedule your appointment.
FAQ AFTER SURGERY
-
When you leave the office there will be a large pressure bandage in place. This consists of a mound of gauze and white elastic tape to prevent bleeding. The area will be numb from the local anesthesia for approximately 2-3 hours after surgery. After the anesthesia wears off, the amount of discomfort is variable. It depends on the site, the size of the defect and closure. Most people feel a little tired/fatigued after the procedure.
-
You CAN go back to work after Mohs surgery; however most people do not. Given the large bandage, post-operative discomfort/fatigue, and our recommendation to apply an ice pack every hour, you may find working that afternoon to be difficult.
-
In order to provide you with the best surgical outcome, we recommend that you do NOT exercise until your stitches are removed. The primary goals during the post-operative period are to 1) minimize stretching of the wound and 2) prevent bleeding in the wound. Stretching of the wound occurs when the skin around the stitches moves (e.g. playing tennis with a wound on your upper back, or climbing stairs with stitches in your leg). Bleeding occurs when your blood pressure and pulse increase with exercise. Taking a walk for example is acceptable as this exertion keeps the blood pressure and heart rate below peak levels.
If you do not have any stitches, there are no restrictions on physical activities after the first 48 hours
-
You should not fly for 48 hours after your surgery. All other travel depends on the surgical site and chosen closure. If stitches are placed, they will need to be removed in 1-2 weeks depending on the site. Ideally, you would be back in town for suture removal. We do understand that some of our patients have very busy travel schedules, and we can absolutely work with you. Please let us know your needs when you schedule your appointment.
-
Starting the day AFTER surgery, it is fine for the stitches to get wet under running water (e.g. showers are fine). However, the stitches should NEVER be immersed or soaked in water for a long period of time (e.g. in a pool). Wet bandages should also be changed immediately.
-
Not around the area that has stitches. For example, if the stitches are on your right cheek, you can shave on the left side and chin. Shaving over the stitches can accidentally cut the stitches and that is something you want to avoid.
-
The two most important things to remember in post operative care are 1) keep the wound free of scabs and 2) keep it lubricated with ointment. The purpose of a band-aid is to keep the ointment on the wound and prevent it from drying out. It is okay to leave the wound uncovered as long as you reapply the ointment every 2-3 hours throughout the day.
-
For over-the-counter pain relief, we recommend that you take Tylenol (acetaminophen)–either 1 extra-strength tablet or 2 regular strength tablets every 6 hours. Please refrain from aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve) as these thin your blood and increase the risk of bleeding. Your surgeon may also provide a prescription pain medication.
-
Research shows that the use of these products yields no significant difference in the cosmetic outcome of your surgery. During the initial wound healing period, keeping the skin lubricated benefits you the most.
-
If it is a life-threatening emergency, call 911. Otherwise, please call us at 650-326-7222. If it is after hours and you need to speak with a physician, please call the same number 650-326-7222. Our answering service will then page the doctor on call.
CUTANEOUS SURGERY
There are times when Mohs surgery is not indicated to remove a lesion. In the consultation, your doctor may recommend other methods of treatment such as: cryotherapy (freezing), curettage and electrodesiccation (scraping and burning with an electric needle), excisional surgery, radiation therapy or "Slow Mohs" surgery.
-
Sometimes lesions on the skin can be removed with a simple excision. For example, the growth may be a benign (not cancerous) lesion such as a cyst. Or the tumor may be located in an area where there is spare tissue, such as the abdomen. In these cases an excision is performed. This procedure typically takes about 30-45 minutes.
-
There are some skin cancers for which we do not recommend Mohs surgery. During traditional Mohs surgery, the tissue is frozen with liquid nitrogen. This quick process is great for identifying some tumors such as basal cell and squamous cell skin cancers. However, this process can make it difficult to identify certain cells and tumors such as melanoma under the microscope. In these cases, we often recommend a modified procedure called “Slow Mohs.”
The surgical part of “Slow Mohs” is exactly the same as regular Mohs surgery except that it is performed over a few days instead of a few hours. Just like Mohs, the surgery is done under local anesthesia in the office. The goals are also the same in that we want to give you the highest cure rate while sparing as much normal tissue as possible. The only difference is that instead of quickly freezing the tissue, it is sent to a lab and placed into a wax block overnight. Microscope slides or "permanent sections" are made the next morning for the dermatopathologist to read. This slow process preserves the identifying features of these tumors so that we can tell if the margins are clear. If cancer is still present, you will return to our office the next day and we will remove only that skin where the cancer remains. Once we are sure that no tumor remains, we will discuss your closure options with you.
With the "Slow Mohs" procedure, we typically reserve several 30-45 minute appointments for you over consecutive days.”
COSMETICS
-
Botox® is a nonsurgical treatments that are FDA approved to temporarily smooth moderate to severe frown lines between the brows. They can also be used to treat wrinkles at other sites such as the forehead and around the eyes. These “dynamic” or “expression” lines are formed in the skin with repeated movement of the underlying muscles.
Botox® injections are purified proteins produced by the Clostridium botulinum bacterium. When injected into a muscle, they reduce that muscle’s ability to contract. This decrease in activity (i.e. decrease in frowning, brow furrowing, squinting, etc.) improves the lines and wrinkles around the muscle.
In our practice, all cosmetic procedures including Botox® injections are performed by physicians.
BEFORE AFTER
-
Over time, the face naturally loses its fullness and volume. This is often first seen around the mouth with deepening nasolabial folds (the curved lines running from the nose to the corner of the mouth) and marionette lines (lines running from the corner of the mouth to the chin or jaw). The lips also lose their fullness creating small vertical lines around the mouth.
Fillers are injected into these areas to restore the volume and fill in the lines. The most common fillers we use in our office are Restylane® and Juvederm®. Each type of filler has its own advantages and disadvantages. Dr. Miller or Dr. Starr will discuss with you which one best suits your needs.
-
We have a Diolite 532nm (KTP) laser in our office. This laser is most often used to treat small broken blood vessels on the face. It also works well for red spots on the body (cherry angiomas), sun spots, freckles, and small seborrheic keratoses.
-
Skin tags are common benign growths most often found on the neck, axilla and groin. They can be easily removed by snip excision, laser, cautery or a freezing treatment (cryosurgery).